Published by The Journal of Child Psychology and Psychiatry, January 2025

RESEARCH OBJECTIVE
Emotional disorders such as depression and anxiety are common in children and young people. If these are not identified or treated then these difficulties can persist into adulthood, increasing the risk of other mental health conditions, poor physical health, self-harm and suicide. This study, led by the School of Medicine at the University of Nottingham and funded by the National Institute for Health and Care Research, set out to explore whether a standardised diagnostic assessment tool could help ensure children and young people get the help they need.
METHOD
The researchers conducted a randomised controlled trial in eight large mental health trusts in England. A total of 1,225 children and young people aged five to 17 years old with emotional difficulties who had been referred to child and adolescent mental health services (CAMHS) were assigned to two groups. The first group completed an online development and wellbeing assessment alongside standard assessment while the second control group just received standard assessment. The children and young people were followed up at six, 12 and 18 months after referral.
KEY FINDINGS
The study found children and young people with high levels of mental health needs were struggling to get the help they need or have their difficulties recognised.
All children and young people included in the study had high levels of mental health needs with more than two thirds – 67% – scoring very high for at least one emotional disorder, most commonly anxiety or depression. However, only 11% received a clinical diagnosis of an emotional disorder from CAMHS within one year of referral.
Only 44% had their referral to CAMHS accepted and 35% were re-referred, suggesting there were delays in getting help.
One year after referral, there was little sign of improvement for most children and young people with both young people and their parents reporting high levels of mental health symptoms including thoughts of self-harm and actual self-harm. At 18 months, 47% had been offered treatment or intervention from CAMHS.
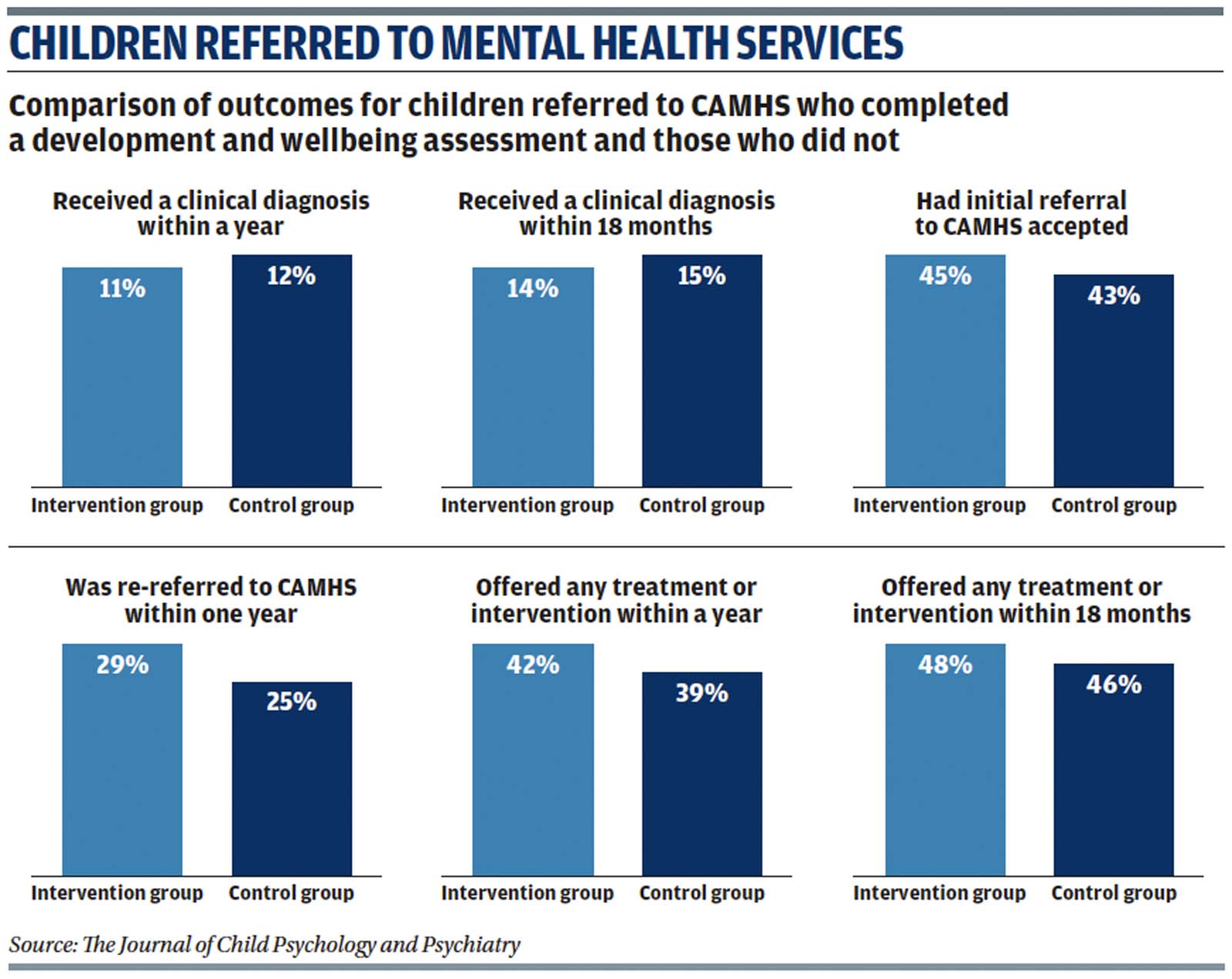
The study found that completing the online standardised diagnostic assessment tool soon after referral did not seem to have an impact on whether a child or young person received a clinical diagnosis or on their clinical outcomes with little difference between the group that did the assessment and the control group. For example, 11% of the intervention group were diagnosed by a clinician within a year compared with 12% of the control group.
IMPLICATIONS FOR PRACTICE
The study highlights the urgent need to reduce delays in access to mental health support. However, there was no evidence to suggest that introducing a standardised diagnostic assessment tool would help ensure problems were identified or treated sooner. The findings show families and young people seemed to like the online approach suggesting it could be a way to offer and increase access to help as long as there was also investment in CAMHS.
AUTHORS
Authors Kapil Sayal, Laura Wyatt, Christopher Partlett, Colleen Ewart, Anupam Bhardwaj, Bernadka Dubicka, Tamsin Marshall, Julia Gledhill, Alexandra Lang, Kirsty Sprange, Louise Thomson, SebastianMoody, Grace Holt, Helen Bould, Clare Upton, Matthew Keane, Edward Cox, Marilyn James, Alan Montgomery
FURTHER READING
Evaluating the Development and Wellbeing Assessment in Paediatric Anxiety and Depression, Paia Amelio and others, Child and Adolescent Psychiatry and Mental Health, January 2024
The Effect of the Development and Wellbeing Assessment as an Adjunct to Standard Referral Letters on Referral Decisions by Child and Adolescent Mental Health Services, Anna Sofie Hansen and others, Clinical Child Psychology and Psychiatry, March 2023
Depression in Children and Young People: Identification and Management, National Institute for Health and Care Excellence, June 2019

