
This has seen staff leave and workers strike over pay and conditions in 2023 with more than 100,000 vacancies across all NHS roles in England.
In June, the government pledged action in its long-term workforce plan for the NHS in England, including doubling doctor and nurse training places by 2031 and improving staff retention through flexible pensions and better career progression. A national framework to fund apprenticeship schemes is also promised.
However, the Royal College of Nursing is concerned about a lack of detail around financial support for student nurses and staff retention in the workforce plan.
Nurses and midwives
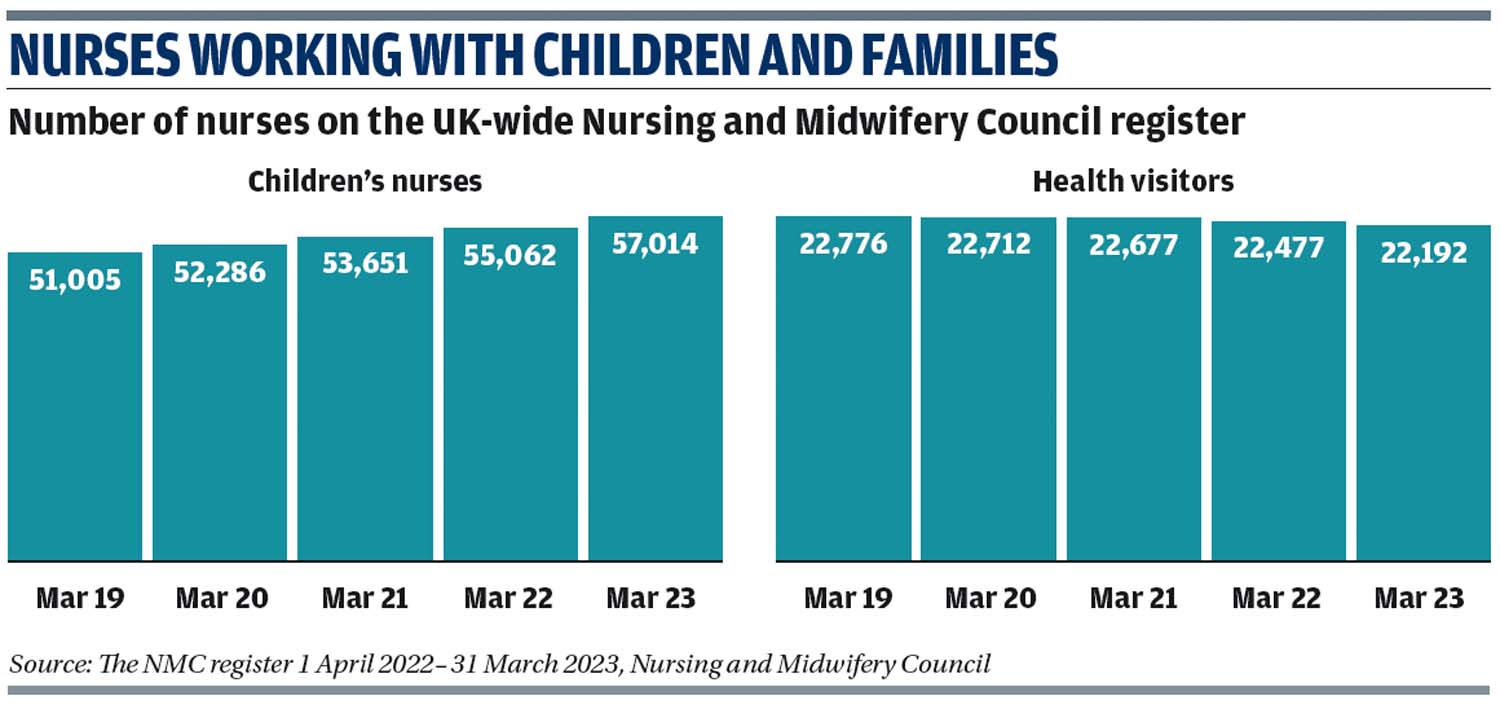
As of March 2023, there were 788,638 nurses, midwives and nursing associates registered with the Nursing and Midwifery Council (NMC). In the year to March 2023, the number of midwives grew from 40,163 to 41,716 and children's nursing numbers rose from 55,062 to 57,014.
But 52 per cent of the 27,000 nurses and midwives who left in 2022/23 did so earlier than planned. Retirement, health concerns and burnout were the main reasons given.
The workforce plan aims to double nurse training places to 38,000 by 2031/32. However, the Universities and Colleges Admissions Service (Ucas) received just 33,750 applications for undergraduate nursing courses by January 2022, compared with 41,220 at the same time in 2021.
Plans to double the school nurse training intake from 335 in 2022 to 662 by 2031 are also included in the NHS workforce plan. Their numbers fell 32 per cent between 2010 and 2022.
Meanwhile, in February the NMC's pre-registration education programme changed to be more flexible, allowing simulated training, such as the use of virtual reality technology, for up to 600 of the 2,300 practice learning hours needed.
The changes also allow greater flexibility in placements to better reflect the wide variety of settings where nurses work, including prisons and social care.
Entry requirements have also been relaxed, to improve access for refugees and those from travelling communities. Applicants no longer need 12 years of evidenced general education.
Last year, the NMC published standards for specialist community public health nurse roles, including school nurses and health visitors, focusing on issues such as children's rights.
Health Education England has launched a blended learning degree in midwifery with training carried out remotely and near to students' homes.
Health Visitors
The NHS long-term workforce plan includes boosting health visitor training intake from 768 in 2022 to 1,339 by 2031.
An Institute of Health Visiting (IHV) survey of the profession found 85 per cent believe there are not enough health visitors and 73 per cent say there is a lack of student health visitor places. Meanwhile, 78 per cent are affected by stress and 62 per cent feel demotivated.
Specialist IHV training courses cover issues such as domestic abuse, nutrition and autism.
Mental health
NHS Digital figures published in November 2022 show 18 per cent of children aged seven to 16 had a probable mental health disorder, up from 12 per cent in 2017.
The government's workforce plan aims to increase training places for mental health nurses, boosting the intake from 5,714 in 2022 to 11,012 by 2031. A 26 per cent increase in clinical psychology and psychotherapy places by 2031 is also in the plan.
In February 2023, Health Education England announced a pilot to train thousands of professionals, including sports coaches, to spot signs of mental health problems among children.
Mental health support teams (MHSTs) have been created to train senior mental health leads within education settings. As of 2022/23, 28 per cent of schools and colleges were covered by an MHST. This is set to rise to 35 per cent by April 2024.
Government grants of £1,200 to schools and colleges to train senior mental health leads are available. The government has committed funding for training up to 2025.
Meet the practitioner

Imogen Boness, health visitor, Cardiff and Vale University Health Board
Imogen Boness' interest in health visiting began when she qualified as a mental health nurse and supported mothers experiencing mental health problems in Cardiff.
“This sparked an enduring interest in perinatal mental health, infant development, and the impact of adverse childhood experiences,” she explains and prompted her to apply for specialist community public health nurse health visitor training.
She qualified as a health visitor last year and through the Institute of Health Visiting is training to be a specialist in perinatal and infant mental health and carrying out emotional wellbeing visits. She is also undergoing Newborn Behavioural Observation training via the Brazelton Centre UK around newborn baby communication and supporting parent and infant relationships.
She wishes she had applied for the health visitor course sooner. “Experience has taught me that I had so many transferable skills as a mental health nurse,” she says.
She says nurses and midwives wanting a career in health visiting should have confidence in their ability to support families.
“I am so glad I built the confidence and went for it. Since qualifying, I have really enjoyed getting to know the area I work in and the families on my caseload,” she adds.

