Research Report: Effectiveness of a Nurse-led Programme for First-time Teenage Mothers
Charlotte Goddard
Tuesday, November 10, 2015
A team of researchers, led by Dr Michael Robling at Cardiff University's School of Medicine, set out to assess the impact of the Family Nurse Partnership programme on outcomes for babies and mothers up to 24 months after birth.
Authors Michael Robling, Cardiff University, and others
Published by The Lancet, October 2015
SUMMARY
The Family Nurse Partnership (FNP) programme offers teenagers expecting their first baby up to 64 structured home visits from a specialist nurse, from early pregnancy until the child is two. Adapted from a US initiative, it was rolled out in England from 2006 in an effort to improve pregnancy outcomes, children's health and development, and parents' economic self-sufficiency.
The researchers recruited a sample of 823 young women taking part in the programme as well as receiving the usual care from health and social services, and 822 who were just receiving the usual care. The young women were all 19 or under and expecting their first baby and from 18 different areas in England. The two groups had comparable demographics including the proportion who spoke English as a first language, ethnic origin, relationship status, employment and education.
Dr Robling and his colleagues tracked the women and children for two years and examined outcomes including smoking by mothers at the end of pregnancy, birthweight, subsequent pregnancies, and emergency hospital attendances and admissions up to the child's second birthday. Findings from the study - Effectiveness of a Nurse-led Intensive Home-visitation Programme for First-time Teenage Mothers (Building Blocks): A Pragmatic Randomised Controlled Trial - were published in medical journal The Lancet this autumn.
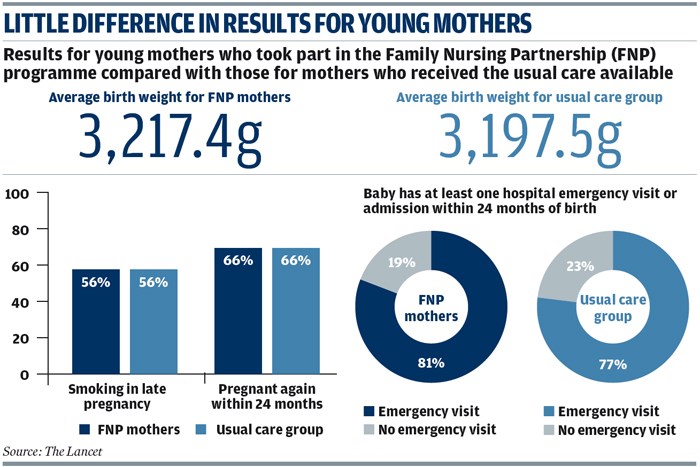
The researchers found the proportion of women who smoked during late pregnancy did not differ between the groups at 56 per cent for both, and neither did the number of cigarettes smoked. The average birthweight was similar at 3,217g in the FNP group and 3,197g in the usual care group. The proportion of children attending or being admitted to hospital in an emergency was also similar at 81 per cent in the FNP group and 77 per cent in the usual care group. In both groups two thirds of women went on to have another pregnancy within two years of having their first child.
Taking part in the FNP programme did show slight positive impacts on outcomes such as intention to breastfeed, early language development, relationship with partners and general self-efficacy. However, the report authors say evidence for a positive impact on child development would mainly show up in children after the age of two years, requiring longer-term follow-up. Rates of child safeguarding concerns were higher for FNP clients than for those not taking part in the programme. The researchers suggest this could be down to higher levels of healthcare contact and nurses adopting a lower threshold for intervention among the FNP group.
The FNP programme was shown to cost around £1,993 per mother.
IMPLICATIONS FOR PRACTICE
The study concludes the FNP programme is not cost-effective when it comes to the primary outcomes of stopping smoking and second pregnancies. Although evaluations of the US programme have shown considerable benefits to those taking part, the researchers suggest teenage parents in England, unlike those in the US, are able to access support from statutory health and social services, which may dilute the impact of the FNP programme in this country.
The report authors say that although the FNP programme cannot be supported on the basis of the trial evidence for its effectiveness in England, any changes to the intervention or to those targeted would justify re-examination. They also say a longer-term follow-up of the current trial cohort may show positive benefits which could shift the balance in favour of the intervention.
FURTHER READING
Community Intervention to Prevent Child Maltreatment in England: Evaluating the Contribution of the Family Nurse Partnership, Kevin Browne and Vicki Jackson, University of Nottingham Medical School, Journal of Public Health, May 2013. This study concludes the FNP programme could be improved by targeting clients with specific risk factors.
Home Visiting by Paraprofessionals and by Nurses: A Randomised, Controlled Trial, David Olds, JoAnn Robinson, Ruth O'Brien and others, Pediatrics, September 2002. An evaluation of the Nurse Family Partnership programme in the US, showing multiple benefits to participants.
The Family-Nurse Partnership Programme in England, Professor Jacqueline Barnes, Mog Ball, Pam Meadows, Beth Howden, Angela Jackson, Juliet Henderson and Lisa Niven, Birkbeck, University of London, published by the Department of Health, January 2011. A report following the first wave of FNP clients and evaluating its benefits.