Patterns of Referral and Waiting Times for Specialist CAMHS
Charlotte Goddard
Tuesday, March 28, 2017
Children and young people's access to timely and appropriate mental health services for addressing their immediate needs as well as preventing long-term problems in adulthood.
Authors Joanna Smith, Richard Kyle, Brigid Daniel and Gill Hubbard
Published by Child and Adolescent Mental Health, February 2017
Report Patterns of Referral and Waiting Times for Specialist CAMHS
SUMMARY
Up to half of mental health disorders in adults begin before the age of 14, according to the World Health Organisation. During a six-month period in 2013, around 6,462 children and young people were referred to Child and Adult Mental Health Services (CAMHS) in Scotland. A quarter of these referrals - 1,608 - were rejected. Researchers at the University of Stirling and Edinburgh Napier University set out to examine whether children and young people have access to timely and appropriate mental health services to address their immediate needs as well as preventing long-term problems in adulthood.
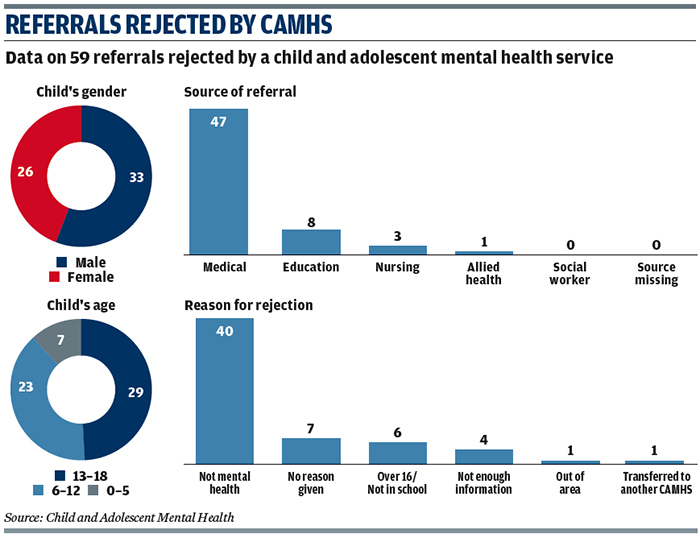
The team analysed the referral forms of 476 children and young people who were referred to CAMHS in one Scottish local authority area between 1 May 2013 and 31 May 2014. More young men than women were referred during this time - 56.3 per cent compared with 43.7 per cent. Older children were more likely to be referred than younger children. Around half - 49.2 per cent - of referrals were adolescents with only 10.1 per cent aged five or under.
The most common reason for referral was emotional and behavioural problems at 30.5 per cent, followed by common mental health disorders at 24.8 per cent and hyperactivity or inattention at 16.4 per cent.
The majority of referrals - 84.7 per cent - were made by a medical professional, mostly a GP (67.4 per cent). The fewest referrals were made by health visitors (0.6 per cent) and social workers (2.1 per cent). However, the researchers say these professionals may have been involved in initial identification of needs or signposting young people to medical professionals.
Of the referrals, 71.8 per cent were accepted for treatment by CAMHS and 12.4 per cent were rejected. The others were either accepted but removed from the waiting list before the start of treatment (13.9 per cent) or were subject to a consultation between the referrer and a CAMHS specialist, the results of which were not tracked.
The main reason for a referral to be rejected was that the issue was recorded as "not mental health", which happened in 68 per cent of cases that were not accepted, followed by the young person being over 16 or not in school (10 per cent of cases). The researchers found children referred for emotional and behavioural problems were more likely to be rejected. Referrals made by education professionals such as teachers were also more likely to be rejected.
The average waiting time for children whose referral had been accepted was 17.9 weeks. The researchers found boys, and those referred for hyperactivity or inattention, were more likely to have longer waiting times while adolescents and those referred with self-harm or eating disorders were more likely to have shorter waiting times.
IMPLICATIONS FOR PRACTICE
Policymakers should look at ways to foster dialogue and collaboration between different groups of professionals making and accepting referrals to CAMHS in order to improve timely access to appropriate mental health support services for children and young people, say the researchers. Initial assessments of children and young people's mental health needs need to be robust, particularly when it comes to referrals for emotional and behavioural problems, so children that require specialist support do not fall through gaps between services.
The report authors say further research is urgently needed to investigate the experiences of children and young people who are either rejected by CAMHS or wait lengthy periods of time before starting their treatment.
FURTHER READING
A Letter of Consequence: Referral Letters from General Practitioners to Secondary Mental Health Services, Ian Shaw and others, Qualitative Health Research, January 2005. An analysis of how GP referral letters fail to meet guidelines and what should be done.
General Practitioner Experience and Perception of Child and Adolescent Mental Health Services (CAMHS) Care Pathways: A Multi-Method Research Study, Saba Hinrichs and others, BMJ Open, January 2012. An investigation of the likelihood of GP referrals to CAMHS being rejected.
Missed Opportunities: A Review of Recent Evidence into Children and Young People's Mental Health, Lorraine Khan, Centre for Mental Health, June 2016. A report which finds that on average children and young people with mental health difficulties go 10 years between first becoming unwell and getting help.




